While the influenza panel coincided with the centennial of the deadly 1918 influenza pandemic (also known as the “Spanish flu”), seasonal influenza epidemics occur every year and kill on about 375,000 people annually. Influenza symptoms vary in severity and can include fatigue, runny nose, fever, and aches. Most people recover within a few weeks. However, certain groups of people are at an elevated risk for influenza complications. The very old and young, as well as people with some chronic health problems are more likely to exhibit severe symptoms and require hospitalization. Most healthy people don’t die of seasonal influenza infections, but they miss work and school, costing society as a whole a lot of money.
The first two panelists were epidemiologists from the Maryland Department of Health (MDH). Brian Bachaus, MS, discussed the flu surveillance programs implemented by the MDH. They monitor influenza and influenza-like illness (ILI) reported at primary care physicians’ offices and emergency departments. MDH also runs a program called the Maryland Resident Influenza Tracking Survey, where volunteers sign up to receive weekly emails prompting them to report ILI symptoms. You can sign up here to volunteer. Mr. Bachaus also described influenza testing at MDH. The state laboratories obtain, sequence, and culture influenza isolates. The results of these monitoring and testing activities are reported weekly during flu season. David Blythe, MD, focused on the role of the MDH in detecting and responding to novel influenza infections. He described a recent example the zoonotic transmission of a novel influenza virus from sick pigs at Maryland agricultural fairs to 40 people. Two children were hospitalized; however, everyone recovered from the infection. Through this case study, Dr. Blythe emphasized the need for a One Health approach; that is, that animal health impacts human health; and that collaborative, multidisciplinary responses are required to protect vulnerable populations from infectious diseases.
The third panelist was Katherine Fenstermacher, Ph.D., from Johns Hopkins Center of Excellence for Influenza Research and Surveillance (JH-CEIRS). JH-CEIRS has three hospital sites in Baltimore, Taiwan, and Zambia. First, Dr. Fenstermacher explained the drawbacks of traditional ILI screening. As you might expect, flu symptoms are non-specific, so without testing, it’s impossible to know if someone is suffering from influenza or a completely different infection. They developed and implemented a screening protocol to streamline ILI screening in the emergency department and to capture patients with mild to severe influenza infections. Second, Dr. Fenstermacher explained the CEIRS research pipeline. The scientists obtain and sequence viral isolates from the JH-CEIRS hospitals. If an influenza isolate is particularly interesting, they produce the virus and test how it interacts with nasal epithelial cells in the lab. For example, the JH-CEIRS scientists can characterize the virulence of the isolate or determine how well the virus can be neutralized by antibodies.
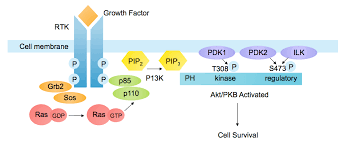
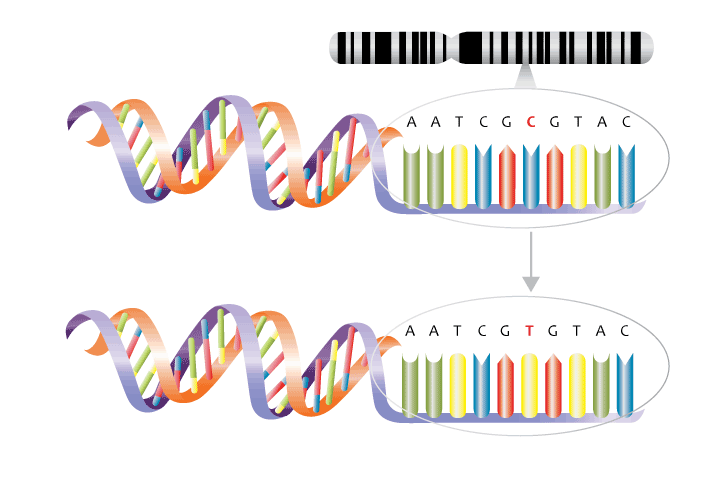
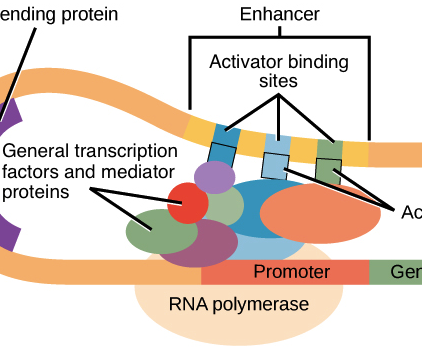
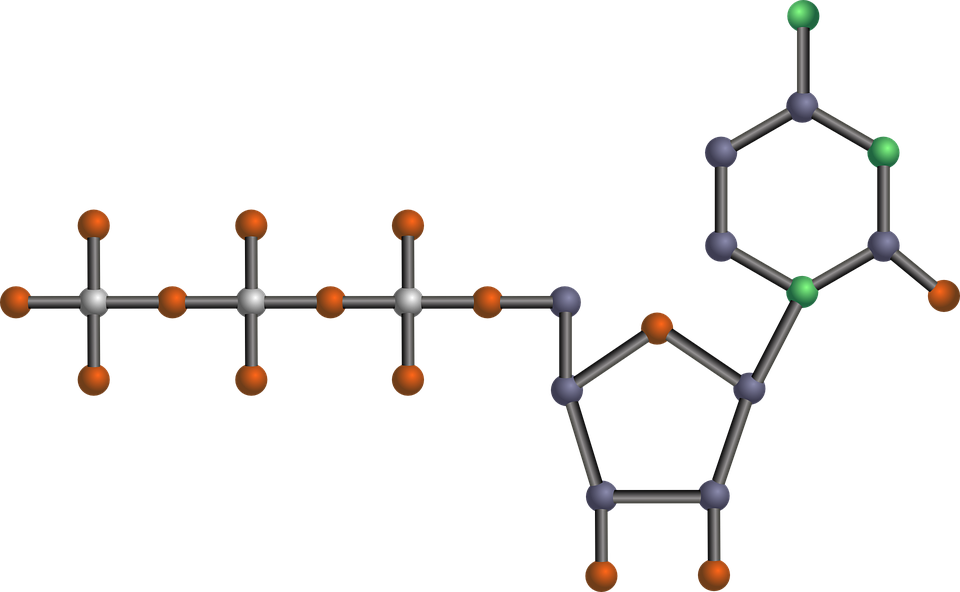
The audience had many questions about how the biology of the influenza virus impacts surveillance, research, and vaccine production. Influenza is an RNA virus with eight segments of RNA that encode essential viral proteins. All eight pieces are required for the viral particle to be fully infectious. Influenza A and B are responsible for most of the human infections. Influenza A is categorized into several subtypes based on the structure of two key surface proteins, hemagglutinin (H) and neuraminidase (N). For example, the predominant influenza A strain that circulated in the Northern Hemisphere last year was H3N2, while the Spanish Flu and the 2009 swine flu outbreak were H1N1 strains. Because influenza A can infect many different animals, including humans, swine, and birds, new influenza A strains can be generated through a process called “reassortment.” For example, if a pig is co-infected with a highly pathogenic pig-specific influenza A virus and a strain that can also infect humans, a highly pathogenic influenza virus that infects humans could result and cause a pandemic. Influenza A also mutates quickly, allowing it to evade the immune system of its host population. Influenza B is responsible for seasonal influenza infections, not global pandemics, and largely infects humans. Type A and B influenza viruses don’t exchange genetic material with each other, although the mechanisms preventing reassortment between the two types are not well understood.
Influenza vaccines are created by growing the virus in embryonated chicken eggs. Unfortunately, scientists must decide which influenza subtypes to include in the vaccine well in advance of flu season because it takes several months to produce, test, and distribute enough vaccines to effectively mitigate the seasonal flu epidemic. Most vaccines administered consist of three or four inactivated virus strains (e.g. two influenza A strains and one influenza B strain), that stimulate the immune system to make antibodies against the antigens present in the dead virus. A small percentage of manufactured vaccines are live attenuated influenza vaccines (LAIVs), which consist of weakened influenza viruses that don’t cause disease but still trigger an immune response. The final panelist, Kawsar Talaat, MD, performs clinical trials on LAIVs at Johns Hopkins Bayview. Her research goal is to develop LAIVs for flu pandemics. Unfortunately, LAIVs overall are generally not as effective as the inactivated vaccines. However, even though the primary antibody response induced by LAIVs is minimal, people are still protected to some extent by LAIVs (e.g. FluMist). Dr. Talaat showed that the LAIV she tested actually triggered a desirable cross-protective memory response, which is not typically induced by the conventional flu shot.
Influenza killed over 80,000 people in the United States during the last flu season. The easiest way to avoid getting the flu this winter is to get vaccinated. Not only are you less likely to get sick, you protect others who either can’t get the vaccine or are at high risk for influenza complications.
Please see these resources on influenza for more information:
Maryland Department of Health
Center for Disease Control
World Health Organization